When Your Labs Are “Normal” — But You Still Don’t Feel Well
If you’ve ever walked out of a medical appointment feeling dismissed, confused, or quietly defeated, you’re not alone.
You went in hoping for answers. You described the bloating that hits after meals, the stomach pain that makes eating stressful, the unpredictable bathroom habits, the fatigue that lingers no matter how much you sleep. Maybe you even mentioned the skin issues, the nausea, the growing list of foods your body suddenly “can’t tolerate.”
Then the labs came back.
“Everything looks normal.”
And somehow, you feel worse — not physically, but emotionally. Because if the tests say you’re fine, what does that mean about the way you feel?
For many people, this is the moment they start questioning themselves.
But here’s the truth that often goes unspoken:
Your symptoms are not imagined.
And “normal” labs do not automatically mean optimal health.
Most reference ranges are based on population averages; not on what supports optimal digestion, energy, or resilience. Being “in range” doesn’t always mean your systems are functioning well — only that they don’t meet criteria for disease.
Why Standard Labs Often Miss Gut Issues
Conventional lab work plays an important role in healthcare. It’s excellent for identifying acute disease, severe deficiencies, or conditions that require urgent medical intervention.
What it’s not designed to do is assess the complex, dynamic ecosystem inside your gut.
Standard blood and stool tests typically:
Look for extreme abnormalities, not subtle dysfunction
Screen for a narrow set of conditions
Focus on disease diagnosis, not functional imbalance
Miss early-stage inflammation or microbial shifts
Your gut, however, doesn’t operate on a pass/fail system.
It responds to:
Microbial balance
Digestive enzyme output
Stomach acid levels
Immune signaling
Inflammatory load
Stress and nervous system input
When those systems are under strain, symptoms show up — even if labs don’t wave a red flag yet.
The Symptoms That Get Dismissed the Most
Many of the most disruptive gut-related symptoms are also the most frequently brushed off or labeled as IBS:
Chronic bloating or abdominal distension
Stomach pain or cramping after meals
Alternating constipation and diarrhea
Persistent nausea or heartburn
Fatigue that doesn’t resolve with rest
Breakouts, rashes, or unexplained skin changes
Food sensitivities that seem to multiply over time
These symptoms are signals — your body’s way of communicating that something deeper is happening beneath the surface.
Why IBS Often Isn’t the Full Answer
IBS is often a diagnosis of exclusion. It describes a pattern of symptoms, not a root cause.
IBS can be a helpful starting point, but without investigating root causes, it often leaves people managing symptoms rather than resolving them
While that label can be validating for some, it often leaves people stuck without clarity or direction. There’s rarely an explanation for why the symptoms are happening — or what to do beyond generic diet advice or symptom management.
For many individuals, IBS becomes a catch-all term that quietly ends the investigation.
But functional nutrition asks a different question:
What’s driving these symptoms in the first place?
Your Symptoms Are Information — Not Inconveniences
In functional nutrition, symptoms are data and not something to silence or override.
Bloating might point to fermentation from microbial imbalance.
Heartburn can be linked to low stomach acid instead of an excess.
Constipation may reflect nervous system dysregulation or poor bile flow.
Fatigue can stem from chronic gut inflammation or immune activation.
When we view symptoms through this lens, they stop feeling random or frustrating and start forming a pattern that can be explored and addressed.
What Functional Gut Testing Looks At (That Standard Tests Don’t)
This is where comprehensive stool testing like the GI-MAP can offer deeper insight.
Unlike conventional tests, functional gut testing is designed to evaluate:
The gut environment
Microbial balance
Digestive capacity
Immune and inflammatory activity
Rather than asking “Is there disease present?” it asks:
How well is your gut actually functioning?
What the GI-Map Can Reveal
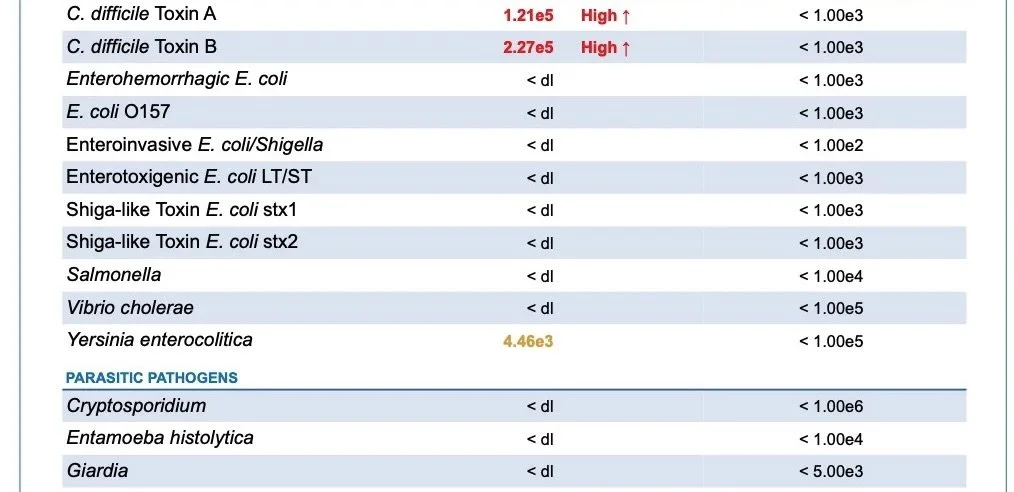
The GI-MAP uses DNA-based technology to identify organisms and markers that often go unchecked in standard testing.
It can uncover:
Parasites and pathogenic bacteria
Even low-level infections can drive bloating, pain, and immune activation.H. pylori overgrowth
A common but often missed contributor to reflux, nausea, nutrient deficiencies, and anxiety.Yeast and fungal imbalances
Frequently linked to bloating, cravings, brain fog, and skin issues.Digestive enzyme and stomach acid markers
Helping explain why food feels like it “just sits” or causes discomfort.Gut inflammation and permeability markers
Providing insight into immune stress, leaky gut patterns, and systemic symptoms.Microbiome patterns associated with IBS, acne, and fatigue
Connecting the dots between digestion, skin, and energy levels.
For many people, this is the first time their symptoms actually make sense.
Why Answers Can Be So Validating
There’s something deeply relieving about seeing your experience reflected on paper.
Not because the results are “bad,” but because they offer context.
They say:
This isn’t in your head
Your body has been communicating all along
There is a reason digestion feels strained
There is a reason you’re exhausted
And most importantly — there is a path forward.
Testing Isn’t About Labels — It’s About Direction
Functional testing can offer valuable insight, supporting deeper understanding and more personalized care.
It can help to:
Guide personalized nutrition strategies
Support targeted supplementation when appropriate
Reduce trial-and-error approaches
Create clarity and confidence in the healing process
Testing doesn’t replace listening to your body — it enhances it.
If You’ve Been Told “Everything is Normal”
If you’ve been brushed off, minimized, or left without answers, please know this:
Your discomfort matters.
Your symptoms are real.
And your body isn’t broken — it’s communicating.
“Normal” labs don’t always mean everything is okay.
Sometimes they simply mean the right questions haven’t been asked yet.
Ready To Understand What Your Gut Is Telling You?
If you’re tired of being dismissed with vague answers and you’re ready to understand what’s actually happening inside your body, you don’t have to figure it out alone.
Follow @greenmindhealth for gut health information
Or book a free consult to explore whether functional gut testing is the right next step for you
Relief starts with better information — and your gut has a story worth listening to.
Sources
Allaband, C., McDonald, D., Vázquez-Baeza, Y., Dorrestein, P. C., Zarrinpar, A., & Knight, R. (2019). Microbiome 101: Studying, analyzing, and interpreting gut microbiome data for clinicians. Clinical Gastroenterology and Hepatology, 17(2), 218–230. https://doi.org/10.1016/j.cgh.2018.09.017
Damhorst, G. L., Adelman, M. W., Woodworth, M. H., & Kraft, C. S (2020). Current capabilities of gut microbiome–based diagnostics and the promise of clinical application. The Journal of Infectious Diseases, 223(Suppl 3), S270–S275. https://doi.org/10.1093/infdis/jiaa689
Dumra, S., & Ray, A. (2025). Recent advances in Helicobacter pylori diagnosis, treatment, and management: A comprehensive review. Exploration of Digestive Diseases, 4, 100598. https://doi.org/10.37349/edd.2025.100598
Istvan, P., Birkeland, E., Avershina, E., Kværner, A. S., Bemanian, V., Pardini, B., Tarallo, S., de Vos, W. M., Rognes, T., Berstad, P., & Rounge, T. B. (2024, February 29). Exploring the gut DNA virome in fecal immunochemical test stool samples reveals associations with lifestyle in a large population-based study. Nature Communications, 15, 1791. https://doi.org/10.1038/s41467-024-46033-0
Mousa, W. K., & Ali, A. A. (2024). The gut microbiome advances precision medicine and diagnostics for inflammatory bowel diseases. International Journal of Molecular Sciences, 25(20), 11259. https://www.mdpi.com/1422-0067/25/20/11259